By Richard Schiffman
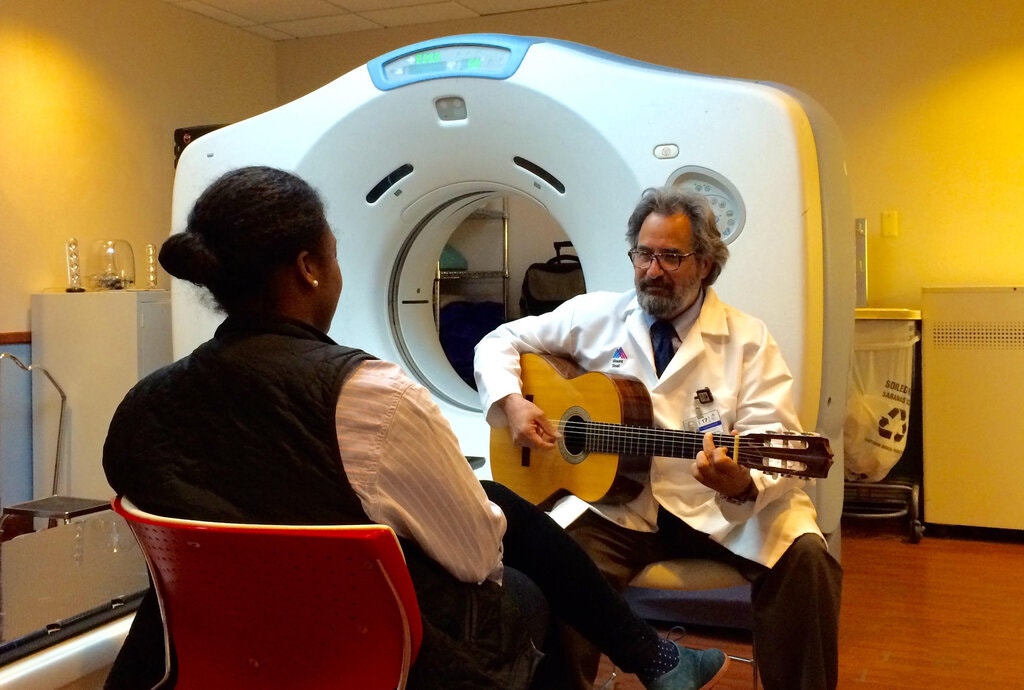
“Focus on the sound of the instrument,” Andrew Rossetti, a licensed music therapist and researcher said as he strummed hypnotic chords on a Spanish-style classical guitar. “Close your eyes. Think of a place where you feel safe and comfortable.”
Music therapy was the last thing that Julia Justo, a graphic artist who immigrated to New York from Argentina, expected when she went to Mount Sinai Beth Israel Union Square Clinic for treatment for cancer in 2016. But it quickly calmed her fears about the radiation therapy she needed to go through, which was causing her severe anxiety.
“I felt the difference right away, I was much more relaxed,” she said.
Ms. Justo, who has been free of cancer for over four years, continued to visit the hospital every week before the onset of the pandemic to work with Mr. Rossetti, whose gentle guitar riffs and visualization exercises helped her deal with ongoing challenges, like getting a good night’s sleep. Nowadays they keep in touch mostly by email.
The healing power of music — lauded by philosophers from Aristotle and Pythagoras to Pete Seeger — is now being validated by medical research. It is used in targeted treatments for asthma, autism, depression and more, including brain disorders such as Parkinson’s disease, Alzheimer’s disease, epilepsy and stroke.
Live music has made its way into some surprising venues, including oncology waiting rooms to calm patients as they wait for radiation and chemotherapy. It also greets newborns in some neonatal intensive care units and comforts the dying in hospice.
While musical therapies are rarely stand-alone treatments, they are increasingly used as adjuncts to other forms of medical treatment. They help people cope with their stress and mobilize their body’s own capacity to heal.
“Patients in hospitals are always having things done to them,” Mr. Rossetti explained. “With music therapy, we are giving them resources that they can use to self-regulate, to feel grounded and calmer. We are enabling them to actively participate in their own care.”
Even in the coronavirus pandemic, Mr. Rossetti has continued to perform live music for patients. He says that he’s seen increases in acute anxiety since the onset of the pandemic, making musical interventions, if anything, even more impactful than they were before the crisis.
Mount Sinai has also recently expanded its music therapy program to include work with the medical staff, many of whom are suffering from post-traumatic stress from months of dealing with Covid, with live performances offered during their lunch hour.
It’s not just a mood booster. A growing body of research suggests that music played in a therapeutic setting has measurable medical benefits.
“Those who undergo the therapy seem to need less anxiety medicine, and sometimes surprisingly get along without it,” said Dr. Jerry T. Liu, assistant professor of radiation oncology at the Icahn School of Medicine at Mount Sinai.
A review of 400 research papers conducted by Daniel J. Levitin at McGill University in 2013 concluded that “listening to music was more effective than prescription drugs in reducing anxiety prior to surgery.”
“Music takes patients to a familiar home base within themselves. It relaxes them without side effects,” said Dr. Manjeet Chadha, the director of radiation oncology at Mount Sinai Downtown in New York.
It can also help people deal with longstanding phobias. Mr. Rossetti remembers one patient who had been pinned under concrete rubble at Ground Zero on 9/11. The woman, who years later was being treated for breast cancer, was terrified by the thermoplastic restraining device placed over her chest during radiation and which reawakened her feelings of being entrapped.
“Daily music therapy helped her to process the trauma and her huge fear of claustrophobia and successfully complete the treatment,” Mr. Rossetti recalled.
Some hospitals have introduced prerecorded programs that patients can listen to with headphones. At Mount Sinai Beth Israel, the music is generally performed live using a wide array of instruments including drums, pianos and flutes, with the performers being careful to maintain appropriate social distance.
“We modify what we play according to the patient’s breath and heart rate,” said Joanne Loewy, the founding director of the hospital’s Louis Armstrong Center for Music & Medicine. “Our goal is to anchor the person, to keep their mind connected to the body as they go through these challenging treatments.”

Dr. Loewy has pioneered techniques that use several unusual instruments like a Gato Box, which simulates the rhythms of the mother’s heartbeat, and an Ocean Disc, which mimics the whooshing sounds in the womb to help premature babies and their parents relax during their stay in noisy neonatal intensive care units.
Dr. Dave Bosanquet, a vascular surgeon at the Royal Gwent Hospital in Newport, Wales, says that music has become much more common in operating rooms in England in recent years with the spread of bluetooth speakers. Prerecorded music not only helps surgical patients relax, he says, it also helps surgeons focus on their task. He recommends classical music, which “evokes mental vigilance” and lacks distracting lyrics, but cautions that it “should only be played during low or average stress procedures” and not during complex operations, which demand a sharper focus.
Music has also been used successfully to support recovery after surgery. A study published in The Lancet in 2015 reported that music reduced postoperative pain and anxiety and lessened the need for anti-anxiety drugs. Curiously, they also found that music was effective even when patients were under general anesthesia.
None of this surprises Edie Elkan, a 75-year-old harpist who argues there are few places in the health care system that would not benefit from the addition of music. The first time she played her instrument in a hospital was for her husband when he was on life support after undergoing emergency surgery.
“The hospital said that I couldn’t go into the room with my harp, but I insisted,” she said. As she played the harp for him, his vital signs, which had been dangerously low, returned to normal. “The hospital staff swung the door open and said, ‘You need to play for everyone.’”
Ms. Elkan took these instructions to heart. After she searched for two years for a hospital that would pay for the program, the Robert Wood Johnson University Hospital in Hamilton, N.J., signed on, allowing her to set up a music school on their premises and play for patients at all stages in their hospitalization.
Ms. Elkan and her students have played for over a hundred thousand patients in 11 hospitals that have hosted them since her organization, Bedside Harp, was started in 2002.
In the months since the pandemic began, the harp players have been serenading patients at the entrance to the hospital, as well as holding special therapeutic sessions for the staff outdoors. They hope to resume playing indoors later this spring.
For some patients being greeted at the hospital door by ethereal harp music can be a shocking experience.
Recently, one woman in her mid-70s turned back questioningly to the driver when she stepped out of the van to a medley of familiar tunes like “Beauty and the Beast” and “Over the Rainbow” being played by a harpist, Susan Rosenstein. “That’s her job,” the driver responded, “to put a smile on your face.”
While Ms. Elkan says that it is hard to scientifically assess the impact — “How do you put a number on the value of someone smiling who has not smiled in six months?”— studies suggest that harp therapy helps calm stress and put both patients and hospital staff members at ease.
Ms. Elkan is quick to point out that she is not doing music therapy, whose practitioners need to complete a five-year course of study during which they are trained in psychology and aspects of medicine.
“Music therapists have specific clinical objectives,” she said. “We work intuitively — there’s no goal but to calm, soothe and give people hope.”
“When we come onto a unit, we remind people to exhale,” Ms. Elkan said. “Everyone is kind of holding their breath, especially in the E.R. and the I.C.U. When we come in, we dial down the stress level several decibels.”
Ms. Elkan’s harp can do more than just soothe emotions, says Ted Taylor, who directs pastoral care at the hospital. It can offer spiritual comfort to people who are at a uniquely vulnerable moment in their lives.
“There is something mysterious that we can’t quantify,” Mr. Taylor, a Quaker, said. “I call it soul medicine. Her harp can touch that deep place that connects all of us as human beings.”